Ketamine has long been associated with party culture, and many on social media brand it simply as a “horse tranquilizer”. So, as more ketamine clinics pop up nationwide, it makes sense that some have confusion about what it is, how it’s made, and where it comes from.
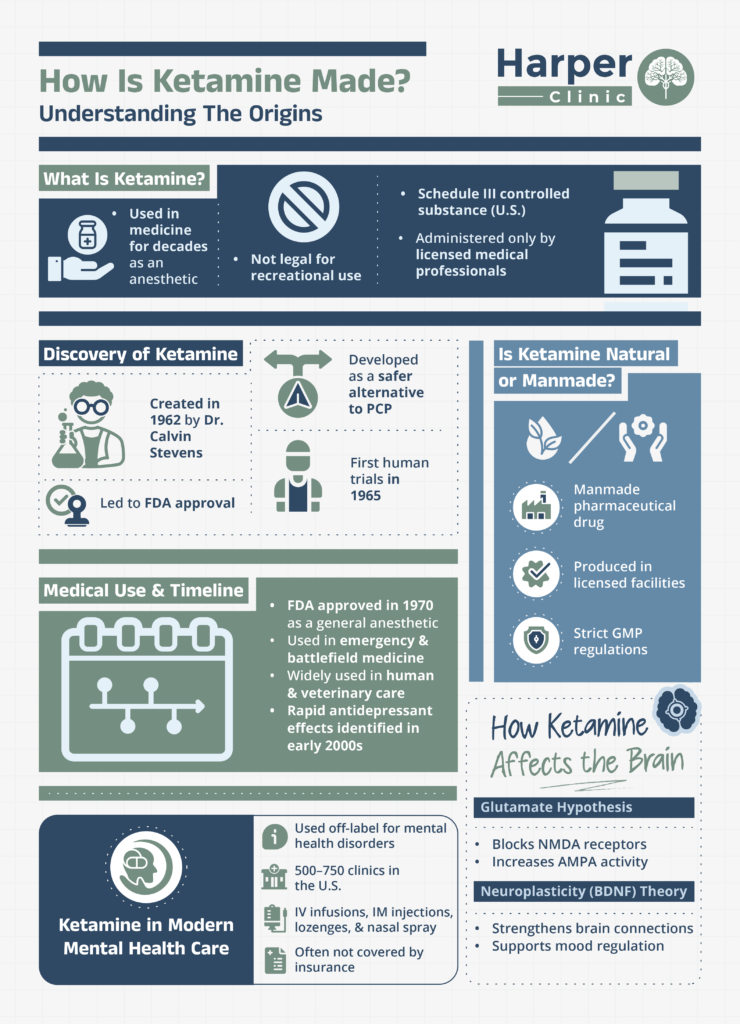
Ketamine has been used in medicine for decades, primarily as an anesthetic. In the US, it is classified as a Schedule III controlled substance. It is not legal for recreational use and can only be administered or prescribed by licensed medical professionals in regulated settings.
In this article, we’ll explore the origins of ketamine and how, over time, it has grown into an effective medical treatment for a variety of conditions.
The Discovery of Ketamine
Ketamine was first made in 1962 by Dr. Calvin Stevens, a chemist at Parke-Davis Laboratories.
His goal was to create a safer anesthetic alternative to phencyclidine (PCP), as PCP is known to cause intense hallucinations and neurotoxicity.
The goal was to develop a compound that provides the anesthetic benefits of PCP, without the adverse side effects, and his research led to the creation of the ketamine molecule. In 1965, Dr. Edward Domino conducted the first human trials on ketamine to observe its dissociative anesthetic effects, eventually leading to FDA approval [1].
Is Ketamine Natural or Manmade?
Ketamine is produced in licensed pharmaceutical manufacturing facilities and synthesized under highly regulated conditions. After synthesis, it undergoes purification and quality control testing to confirm its identity, potency, and safety. Regulatory agencies require detailed documentation, inspections, and compliance with Good Manufacturing Practices (GMP) [1][2].
The molecular (chemical) formula for ketamine is made up of carbon, hydrogen, chlorine, nitrogen, and oxygen. The synthesis of ketamine is a complex chemical process that involves cyclohexanone, a petroleum-derived chemical compound. Through a variety of reactions, including condensation of o-chlorobenzonitrile, the molecule ketamine is made [2].
When Was Ketamine First Used in Medicine?
Ketamine was approved by the U.S. Food and Drug Administration (FDA) in 1970 for use as a general anesthetic. Its ability to provide pain relief and dissociation without significantly suppressing breathing or heart function made it especially valuable in emergency and high-risk settings.
Soon after approval, ketamine became widely used in both human and veterinary medicine. It was commonly used during emergency surgeries, trauma care, and on the battlefield during the Vietnam War. Its reliability, quick onset, and lower impact on the cardiovascular system made it a preferred option in unpredictable environments or with limited resources [1].
In the early 2000s, ketamine gained new attention as research showed its rapid antidepressant effects, especially for individuals with treatment-resistant depression. Ongoing research eventually led to the 2019 FDA approval of esketamine (Spravato), a nasal spray derived from ketamine, for depression [3].
Some of the medical uses of ketamine in clinical settings have included:
- General anesthesia (human and vet medicine)
- Emergency and trauma care
- War, battlefield, and disaster medicine
- Pain management
- Sedation for procedures
- Major depressive disorder and treatment-resistant depression (esketamine)
Medical History Timeline of Ketamine
| Early 1960s | Ketamine is developed as an anesthetic compound |
| Mid 1960s | First human clinical trials begin |
| 1970 | FDA approved ketamine as a general anesthetic |
| 1970s to 1990s | Widespread use of ketamine in surgery, emergency use, and battlefield medicine |
| Early 2000s | Research identifies the rapid antidepressant effects of ketamine |
| 2019 | FDA approves esketamine (Spravato) nasal spray for depression |
Ketamine and Advancements in Brain Health: Current Theories
The use of ketamine has come a long way over the decades, and new technology in neuroscience has helped researchers learn more about how ketamine affects the brain and body, especially when it comes to treating mental health problems.
Although this field is still relatively new and research is constantly evolving, there are currently two main theories that attempt to explain the effects of ketamine on the brain. Rather than only focusing on chemical imbalances, these suggest that brain connectivity, learning, and adaptation may play a bigger role in treating a mental health condition such as depression.
1. The Glutamate Hypothesis
This is the most widely accepted theory and explains how ketamine works differently from traditional antidepressants by targeting the brain’s glutamate system rather than serotonin or dopamine.
This theory says that ketamine blocks NMDA receptors, leading to a quick increase in glutamate activity at AMPA receptors. It is thought to improve communication between brain cells, which may explain why ketamine can reduce symptoms of depression much faster than conventional medications [4].
2. The Neuroplasticity (BDNF) Theory
A second growing theory focuses on neuroplasticity, the brain’s ability to form and repair connections. Research suggests that ketamine activates pathways involving BDNF (brain-derived neurotrophic factor) and mTOR, which are associated with the growth and strengthening of the brain’s synaptic connections.
This may help “reset” neural circuits affected by chronic stress, trauma, or depression, supporting mood regulation and cognitive flexibility [5].
How Is Ketamine Used in Modern Mental Health Care?
Today, ketamine is used off-label by clinicians across the United States for a range of mental health disorders, including major depression, anxiety, obsessive-compulsive disorder, post-traumatic stress disorder, and other treatment-resistant conditions.
Recent data shows there are roughly 500 to 750 ketamine clinics throughout the United States.
These clinics differ in how they administer treatments, from intravenous infusions in a clinical setting to take-home lozenges. Most require patients to pay out-of-pocket, as standard health insurance typically does not cover off-label ketamine for mental health [6].
Breakthrough Ketamine Therapy for Treatment-Resistant Depression
If you’ve already tried conventional methods of mental health treatment with no relief, ketamine may be an ideal option for you. At Harper Clinic Utah, we provide personalized treatment planning and licensed ketamine therapy to address deep-rooted depression, trauma, and emotional blocks.
We require clients receiving ketamine therapy to also be in traditional therapy, either with one of our therapists or an outside provider. Contact our consultation team to learn if you are a good candidate for ketamine assisted therapy today.
Sources
[1] Mion, G. 2017. History of anaesthesia. The ketamine story – past, present, and future. European Journal of Anesthesiology.
[2] Zekri, N. et al. 2020. Synthesis of ketamine from a nontoxic procedure: a new and efficient route. Journal of Chemical Sciences.
[3] Vlisides, P. E. (2016). Ketamine: 50 Years of Modulating the Mind. Frontiers in human neuroscience, 10, 612.
[4] Mason, G. et al. (2018). The effects of ketamine on prefrontal glutamate neurotransmission in healthy and depressed subjects. Official publication of the American College of Neuropsychopharmacology, 43(10), 2154–2160.
[5] Pardossi, S. et al. 2024.Variations in BDNF and Their Role in the Neurotrophic Antidepressant Mechanisms of Ketamine and Esketamine: A Review. International Journal of Molecular Sciences.
[6] Megli, D. 2024. The ketamine economy: New mental health clinics are a ‘Wild West’ with few rules. NPR.